Diagnostic ultrasound systems are now imperative to the medical field. Hitachi Group has newly developed a technology called Vector Flow Mapping (VFM) which displays the intricate details of intracardiac blood flow in a visual and simple manner. In order to commoditize this new diagnostic ultrasound system that uses this technology, we needed to test its reliability. This is where we decided to conduct verification tests with experimental devices that is true to anatomy, and also developed a mechanism to display the precision of the measured data. The desires of researchers who pursue reliability are supporting the medical field.

TANAKA Tomohiko
Senior Researcher

ASAMI Rei
Researcher
(Publication: June 6, 2018)
ASAMIThe form of ultrasound diagnosis that is most familiar to people is probably looking at fetuses inside the uterus of expecting mothers. From an engineering standpoint, it transmits ultrasound waves, that is, sound waves at a frequency much higher than the sound waves emitted when we speak, receives the echoes that return from the inside the body as a reflection, and turn them into the image. Some of the advantages of diagnoses that utilize ultrasound energy are that the effects it has on body are extremely low relative to radiation measurements, that the apparatus itself is small so they can be stored even in small clinics, and that it allows people to view inside body on the spot.
The application developed on this occasion is a system that will diagnose the heart. The heart is an organ that moves at an extremely high rate, and diagnostic systems that utilize ultrasound are extremely useful because they can capture the heart's motion in real time and can provide a diagnosis by quantifying the characteristics.
TANAKADiagnostic ultrasound systems fire ultrasonic beams in a radial pattern from probes one at a time and scan organs to grasp an image of entire organs. Conventionally, utilizing the principle called the Doppler effect, which states that when we pass by an ambulance the sound we hear changes because the frequency of the noise changes, the velocity of blood flow is measured by changes in the frequency of a sound on the beam's trajectory. Generally, the blood flow toward the probe is shown in red and flow away from probe is shown in blue. Using this method, we can tell that there is a blood flow, but we are not able to detect the details of the blood flow, such as the presence of vortices or how they are spinning. This is where we developed a technology called Vector Flow Mapping which displays blood flow information intuitively and in great detail, commercializing the world's first new diagnostic application. VFM utilizes the physical law of the conservation of mass to estimate the components that will be perpendicular to ultrasonic beams, and by displaying complex blood flows with vector arrows, it allows people to visually grasp the direction of blood flow.
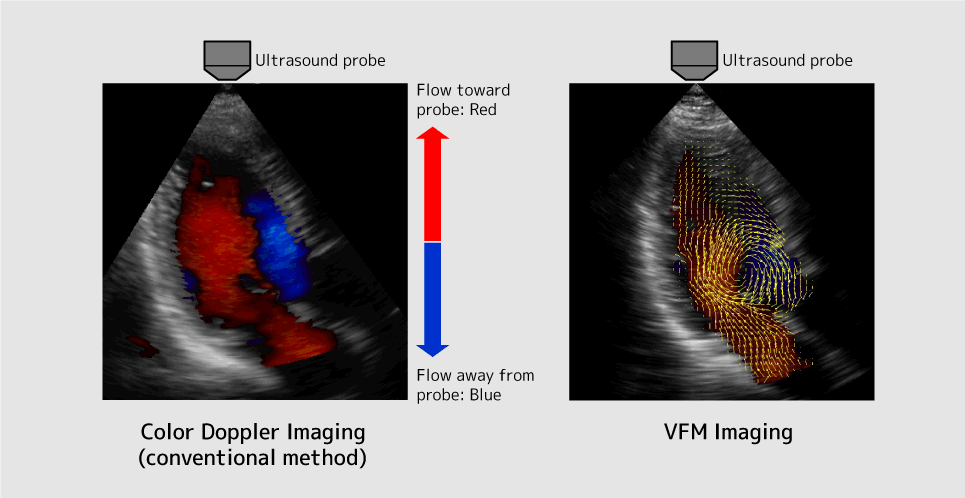
Figure 1: Blood Flow Display Example for Color Doppler (conventional method) and VFM
TANAKAWe are aiming for more detailed diagnoses of cardiac failure. We believe that this will be a method that meets the demands of doctors who wish to forecast scenarios of patients with cardiac failure and conduct diagnoses on patients with relatively unique cases of cardiac failure. For example, because it is difficult to predict the prognosis of a patient, patients who are hospitalized for cardiac failure often return with similar conditions soon after they are discharged. It is anticipated that carefully examining cardiac blood flow vortices of patients using VFM before discharge will help make predictions about prognoses. In fact, some examples have been confirmed, and we are currently verifying whether this method is truly effective.
ASAMIWe were mainly involved in testing the reliability of VFM. In order to commercialize VFM, it was imperative to check whether the values calculated with VFM's algorithms were actually correct and to test if they were reliable. Shortly after Dr. Tanaka launched the project, I joined as well.

ASAMIIn order to examine if the direction of the arrows calculated with VFM coincided with the observed results, we built experimental devices to test the precision and demonstrated the results. Generally, verification methods measure things in an entirely different way because when objects are measured in the same way, the same error sources may recur. Because VFM utilizes the data of sound (ultrasound), we utilized lasers (light) to measure observations.
The experimental device, "a transparent heart," was made based on three-dimensional data of an actual person's heart. In order to create a heart that was as similar to a living human's heart as possible, for the mitral valve in the left ventricle that sends out blood to the entire body, we used an artificial heart valve utilized in medical practice for things such as valve replacements. We also made it so the transparent heart would beat, just as real hearts beat.
Next, we measured both sound and light at the exact same time on the exact same cross section and compared the results of sound calculated with VFM with the results of actual flow observed with the light. As a result, we confirmed that they coincide at a high level of precision.
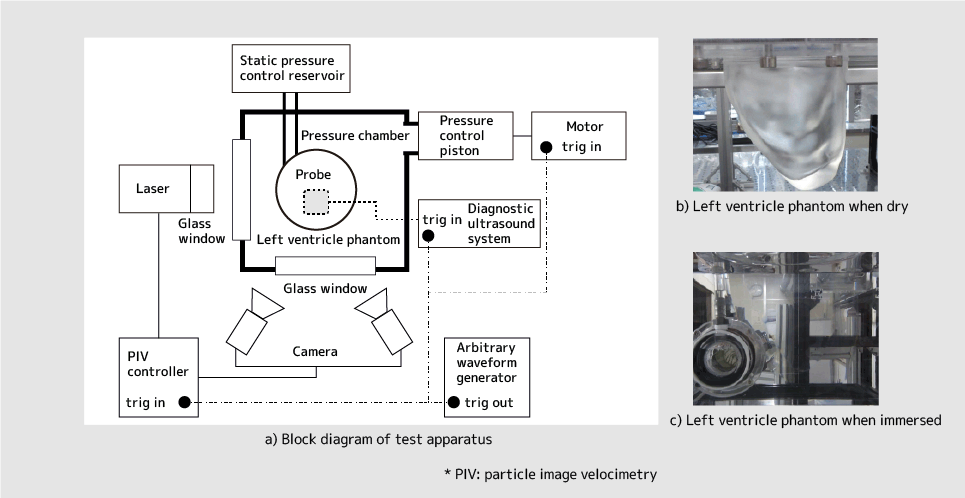
Figure 2: Overview of Experimental Device with the Purpose of Testing VFM Reliability
TANAKABefore we started this research, whether or not VFM calculated values were accurate was a point of debate between involved parties, so much so that it was like air combat. This is where I thought, "seeing is believing" and decided to show them the results. Because the most trusted velocimetry is laser velocimetry, I thought that if I could prove that VFM was accurate using the method that people perceive to be most correct, then they would be convinced.
TANAKACompletely removing optical refraction was difficult. When you place chopsticks inside a glass of water, the chopsticks appear distorted. This is because the refractive index of the air and the water are different. If we conducted the experiments under these conditions, we thought that the precision would decrease, so we calibrated the entire refractive index of the material of the transparent heart and the liquid inside. Because the refractive index of the material was 1.47, Ms. Asami found a liquid that had the same refractive index, and in the end, we finished the transparent heart. Just when I had started worrying about what material to select to make it completely transparent, Ms. Asami chose one in a flash!
TANAKAIn all honesty, I just thought, the numbers correspond quite well! This is mainly because, from a fluid mechanics expertise standpoint, I had substantial doubts that the results calculated by VFM's algorithm wouldn't correspond with the measured values. Despite this, I was involved in testing VFM's reliability because if some people thought that VFM would benefit medicine, then it was my mission to quantitatively evaluate whether it would truly be useful.
ASAMIWhen we presented the results at an academic conference, some professors who specialize in fluid mechanics commented saying, "Your results surprisingly matchup." Until then, there had been some negative opinions, and it was almost as if the tables had turned and I felt as though all of my hard work was validated. I believe the fact we, the people in charge, could say with confidence, "This product should work," played a large role in deciding upon the commercialization of VFM.
TANAKAYes, however, I also thought that even this was not sufficient. This is because the three-dimensional aspect of blood flow could be a source for error in VFM. Blood flow crossing the cross-section being measured can be a source of degradation in precision. Therefore, even if we verify with a transparent heart, there is an issue that errors vary depending on cases with different conditions. Because of this, we derived an algorithm that estimates the precision of measurement through statistical analysis, etc., no matter how the cross-section changes.
ASAMIDr. Tanaka is explaining this rather plainly, but it is actually amazing. The transparent heart mimics healthy adult hearts. However, in reality, VFM could be used for a variety of cases such as unhealthy adult hearts, hearts belonging to elderly people, and hearts of children with heart diseases. Moreover, the cross-section where the heart is examined changes from one occasion to another depending on how the doctors and technicians choose to aim the echoes. The transparent heart only tested one scenario, but this algorithm can display the likelihood of precision in any situation. We thought that this was absolutely necessary.
TANAKAThat's correct. We made it so that it can display how precise the measurements are as auxiliary information. This is when I first felt that "this product could work."
TANAKAI believe so. In conducting collecting data, there is always the chance that you might have errors depending on how it is measured and other conditions. When the reliability of the data is low, the VFM is made so that it alerts the person conducting measurements.

TANAKAHmm…I think what truly makes me happy is when VFM is used to make a correct judgement, and this ends up resulting favorably for the patient. Signs that indicate this are just starting to appear. Some doctors are telling us that their patient prognoses have improved, which means that our true research results are still coming in. Once we have conclusive evidence and data which says that VFM can improve prognoses by X%, then I think I will be able to truly feel good for the first time.
ASAMICurrently, we are in a phase of growing, meaning that we are trying to have this technology properly appreciated at academic conferences. This phase is far from complete.
TANAKAPrecisely. We are currently in the midst of testing VFMs at many facilities. As a future outlook, we hope that this technology will provide some form of a clear benefit for patients, and I believe this is one of my goals for VFM.
TANAKAI hope so. I believe the ultimate reward for researchers is when their research somehow becomes valuable to the world.
ASAMIOf course, I am happy that this system will help people, however this system does not utilize an algorithm that I came up with, thus my current motivation is to create an algorithm and see it go out into the world and help patients.